What is a hysterectomy?
A hysterectomy is the surgical removal of the uterus. Different portions of the uterus, as well as other organs, may be removed at the same time.
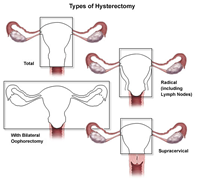
The types of hysterectomy include:
-
Total hysterectomy. Includes the removal of the entire uterus, including the fundus (the part of the uterus above the openings of the fallopian tubes) and the cervix, but not the tubes or ovaries. This is the most common type of hysterectomy.
-
Hysterectomy with salpingo-oophorectomy. Includes the removal of one or both ovaries, and the fallopian tubes, along with the uterus.
-
Radical hysterectomy. Includes the removal of the uterus, cervix, the top portion of the vagina, most of the tissue that surrounds the cervix in the pelvic cavity, and may include the removal of the pelvic lymph nodes. This is done in some cases of cancer.
-
Supracervical hysterectomy (partial or subtotal hysterectomy). Removal of the body of the uterus while leaving the cervix intact
In addition to the different types of hysterectomies, there are different surgical techniques used to perform a hysterectomy. Surgical hysterectomy techniques include:
-
Abdominal hysterectomy. The uterus is removed through the abdomen via a surgical incision about six to eight inches long. This procedure is most commonly used when the ovaries and fallopian tubes are being removed, when the uterus is enlarged, or when disease has spread to the pelvic cavity, as in endometriosis or cancer. The main surgical incision can be made either vertically, from the navel down to the pubic bone, or horizontally, along the top of the pubic hairline.
-
Vaginal hysterectomy. The uterus is removed through the vaginal opening. This procedure is most often used in cases of uterine prolapse, or when vaginal repairs are necessary for related conditions. No external incision is made, which means there is no visible scarring.
-
Laparoscope-assisted vaginal hysterectomy/robot-assisted laparoscopic hysterectomy. Vaginal hysterectomy is performed with the aid of a laparoscope, a thin, flexible tube containing a video camera. Thin tubes are inserted through tiny incisions in the abdomen near the navel. The uterus is then removed in sections through the laparoscope tube or through the vagina. In a robot-assisted laparoscopic hysterectomy, the doctor inserts the laparoscope and other instruments, then uses a computer station to control the instruments.
The type of hysterectomy performed and the technique used to perform the procedure will be determined by your doctor, based on your particular situation.
For women who have not yet reached menopause, having a hysterectomy means that menstruation will no longer occur, nor will pregnancy be possible.
What are female pelvic organs?
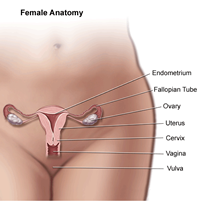
The organs and structures of the female pelvis are:
-
Endometrium. The lining of the uterus.
-
Uterus (also called the womb). The uterus is a hollow, pear-shaped organ located in a woman's lower abdomen, between the bladder and the rectum. The uterus sheds its lining each month during menstruation, unless a fertilized egg (ovum) becomes implanted and pregnancy follows.
-
Ovaries. Two female reproductive organs located in the pelvis in which egg cells (ova) develop and are stored, and where the female sex hormones estrogen and progesterone are produced.
-
Cervix. The lower, narrow part of the uterus located between the bladder and the rectum, forming a canal that opens into the vagina, which leads to the outside of the body.
-
Vagina (also called the birth canal). The passageway through which fluid passes out of the body during menstrual periods. The vagina connects the cervix and the vulva (the external genitalia).
-
Vulva. The external portion of the female genital organs.
-
Fallopian tube. Two thin tubes that extend from each side of the uterus, toward the ovaries, as a passageway for eggs and sperm.
Reasons for the procedure
Reasons for performing a hysterectomy include, but are not limited to, the following:
-
Fibroid tumors. Nonmalignant tumors.
-
Endometriosis. A condition in which endometrial cells grow outside of the uterus, attaching themselves to other organs in the pelvic cavity, resulting in chronic pelvic pain, pain during sex, and prolonged or heavy bleeding.
-
Abnormal uterine bleeding. This is often due to endometrial hyperplasia, an over thickening of the uterine lining that may cause abnormal bleeding.
-
Cancer. Cervical, ovarian, or endometrial cancer is the diagnosis in approximately 10 percent of hysterectomies.
-
Blockage of the bladder or intestines by the uterus or a growth
Hysterectomy may also be performed when uterine prolapse (the uterus drops down into the vagina) occurs, or in the presence of chronic pelvic conditions, such as pelvic pain or pelvic inflammatory disease, that do not respond to other treatments.
There may be other reasons for your doctor to recommend a hysterectomy.
Risks of the procedure
As with any surgical procedure, complications may occur. Some possible complications include, but are not limited to, the following:
-
Hemorrhage
-
Injury to the ureters (tubes that carry urine from the kidneys to the bladder) and urinary bladder
-
Infection
-
Injury to the bowel or other intestinal organs
-
Difficulty with urination or urinary incontinence
Women who have not reached menopause prior to a hysterectomy may experience menopausal symptoms such as hot flashes, mood swings, and vaginal dryness after the procedure if the ovaries are removed. Women will no longer have menstrual periods after a hysterectomy.
Mood swings, depression, and feelings of loss of sexual identity may occur after hysterectomy.
There may be other risks depending on your specific medical condition. Be sure to discuss any concerns with your doctor prior to the procedure.
Before the procedure
-
Your doctor will explain the hysterectomy procedure to you and offer you the opportunity to ask any questions that you might have.
-
You will be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if something is not clear.
-
In addition to a complete medical history, your doctor may perform a complete physical examination to ensure you are in good health before undergoing the procedure. You may undergo blood tests or other diagnostic tests.
-
You will be asked to fast for eight hours before the procedure, generally after midnight.
-
If you are pregnant or suspect that you may be pregnant, you should notify your health care provider.
-
Notify your doctor if you are sensitive to or are allergic to any medications, iodine, latex, tape, or anesthetic agents (local and general).
-
Notify your doctor of all medications (prescription and over-the-counter) and herbal supplements that you are taking.
-
Notify your doctor if you have a history of bleeding disorders or if you are taking any anticoagulant (blood-thinning) medications, aspirin, or other medications that affect blood clotting. It may be necessary for you to stop these medications prior to the procedure.
-
You will be given instructions on how to cleanse your bowels before the operation.
-
You may be told to avoid using a douche and tampons on the day of the procedure.
-
You will be sedated before being taken to the operating room and you will be asleep for the procedure.
-
You may be given an antibiotic to take the day before the procedure.
-
Arrange for someone to help around the house for a week or two after you are discharged from the hospital.
-
Based on your medical condition, your doctor may request other specific preparation.
During the procedure
Hysterectomy generally requires a stay in a hospital. Procedures may vary depending on your condition and your doctor's practices.
The procedure will vary depending on the type of procedure and surgical technique used.
Generally, a hysterectomy follows this process:
-
You will be asked to remove any jewelry or other objects that may interfere with the procedure.
-
You will be asked to remove clothing and be given a gown to wear.
-
If there is excessive hair at the surgical site, it may be clipped off.
-
An intravenous (IV) line will be inserted in your arm or hand.
-
You will be positioned on the operating table lying on your back. For a vaginal procedure, your feet will be placed in stirrups.
-
The anesthesiologist will continuously monitor your heart rate, blood pressure, breathing, and blood oxygen level during the procedure.
-
A catheter (thin, narrow tube) will be inserted into your bladder to drain urine.
Abdominal hysterectomy
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
The incision will be made vertically from the navel to the pubic bone or horizontally across the lower abdomen. The surgeon will discuss which incision is preferable in your particular situation prior to the procedure.
-
After the incision has been made through the layers of skin, muscle, and other tissue, the doctor will inspect the organs and other structures in the abdomen and pelvis.
-
The tissues connecting the uterus to blood vessels and other structures in the pelvis will be carefully cut away.
-
The uterus will be removed, along with any other structures such as the ovaries, fallopian tubes, and cervix, as required by your situation.
-
The incision will be closed with surgical stitches or staples.
Vaginal hysterectomy
-
The lower abdomen and perineum will be cleansed with an antiseptic solution. The rectum may be packed with an antiseptic-soaked sponge.
-
A speculum will be inserted into your vagina to spread the walls of the vagina apart to expose the cervix.
-
An incision will be made inside the vagina, near the cervix.
-
The tissues connecting the uterus to blood vessels and other structures in the pelvis will be carefully cut away.
-
The uterus will be removed through the vagina. If required, excess vaginal tissue and/or other tissue or structures may be removed.
-
The opening into the peritoneal cavity created by the removal of the uterus will be closed with stitches.
Laparoscope-assisted vaginal hysterectomy
-
The skin over the surgical site will be cleansed with an antiseptic solution.
-
A small incision will be made in the abdomen near the navel. Carbon dioxide gas will be introduced into the abdomen to inflate the abdominal cavity so that the uterus and surrounding organs can be more easily visualized. Depending on the type of laparoscope used, additional incisions may be made in the abdomen to accommodate other surgical instruments.
-
The operating table will be tilted so that your head is lower than your feet. This helps to move the other abdominal organs and structures out of the surgical field and make room for the laparoscopic surgical instruments.
-
The laparoscope will be inserted through the incision and the abdominal cavity will be examined. The tissues surrounding the uterus will be removed.
-
Once it is detached from the surrounding tissues, the uterus will be removed through the vagina or through the laparoscope. Other organs or structures, such as the ovaries and/or fallopian tubes, may be removed, depending on your particular situation.
-
When the procedure is completed, the laparoscope will be removed.
Procedure completion, all methods
-
The uterus and any other organs or tissues removed will be sent to the lab for examination.
-
Any skin incision(s) will be closed with stitches or surgical staples.
-
A sterile bandage or dressing or adhesive strips will be applied to skin incisions. A sanitary pad will be applied to the perineal area to absorb any drainage from the vagina.
After the procedure
In the hospital
After the procedure, you will be taken to the recovery room for observation. Your recovery process will vary depending on the type of procedure performed and the type of anesthesia that is given. Once your blood pressure, pulse, and breathing are stable and you are alert, you will be taken to your hospital room.
Abdominal cramping may occur after the surgery. You may receive pain medication as needed, either by a nurse or by administering it yourself through a device connected to your intravenous line.
If your procedure was an abdominal hysterectomy, you may have a thin, plastic tube inserted through your nose into your stomach to remove air that you swallow. The tube will be removed when your bowels resume normal function. You will not be able to eat or drink until the tube is removed.
You may have small to moderate amounts of vaginal drainage for several days. The nurse will check the sanitary pads periodically to monitor the amount of drainage.
You will be encouraged to get out of bed within a few hours after a vaginal procedure or by the next day after an abdominal procedure. In addition, you should perform coughing and deep breathing exercises as instructed by your nurse.
Depending on your situation, you may be given liquids to drink a few hours after surgery. Your diet may be gradually advanced to more solid foods as tolerated.
Arrangements will be made for a follow-up visit with your doctor, usually several weeks after the procedure.
At home
Once you are home, it is important to keep the incision clean and dry. Your doctor will give you specific bathing instructions. If stitches or surgical staples are used, they will be removed during a follow-up office visit, if they were not removed prior to your discharge from the hospital. If adhesive strips are used, they should be kept dry and generally will fall off within a few days.
The incision and the abdominal muscles may ache, especially after long periods of standing. If a laparoscope was used, you may experience shoulder pain from the carbon dioxide in your abdomen. Take a pain reliever for soreness as recommended by your doctor. Aspirin or certain other pain medications may increase the chance of bleeding. Be sure to take only recommended medications.
Walking and limited movement are generally encouraged, but strenuous activity should be avoided. Your doctor will instruct you about when you can return to work and resume normal activities.
Avoid becoming constipated by including fiber and plenty of liquids in your diet. Your doctor may recommend a mild laxative.
If a laparoscopic procedure was performed, you should avoid drinking carbonated beverages for one to two days after the procedure. This will help minimize the discomfort associated with the carbon dioxide gas. In addition, drinking carbonated beverages may cause nausea.
You should not use a douche, tampons, engage in sexual intercourse, or return to work until your doctor advises you to do so.
Notify your doctor to report any of the following:
-
Fever and/or chills
-
Redness, swelling, or bleeding or other drainage from the incision site(s)
-
Increased pain around the incision site(s)
-
Abdominal pain, cramping, or swelling
-
Increased vaginal bleeding or other drainage
-
Leg pain
Following a hysterectomy, your doctor may give you additional or alternate instructions, depending on your particular situation.
Online resources